There are a variety of non-clinical factors that keep your members from getting the care they really need. Learn more about why SDOH should be a priority for your company this year.
Searches for “social determinants of health” have swelled tremendously since the early 2000s, and for good reason. But what exactly are social determinants of health?
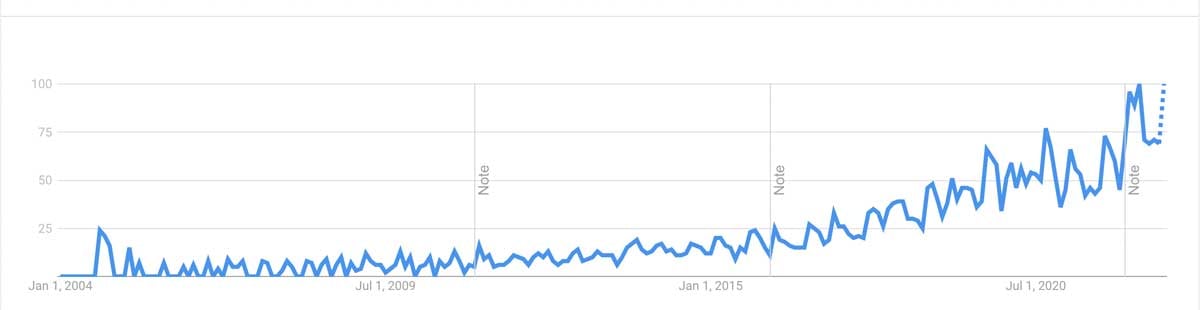
This is a graph that shows search frequency and interest for “social determinants of health” from 2004 to the present.
Some real-life examples of social determinants of health are:
- Your grandmother is unable to get to her primary care doctor on a regular basis because she had to surrender her driver’s license and doesn’t have another mode of transportation.
- Your friend was recently laid off from their position and no longer has health insurance to get their insulin refilled to manage their diabetes.
Both of these examples paint a picture of the impact that non-clinical variables have on one’s health, and those are what social determinants of health (SDOH) are.
As defined by the Department of Health and Human Services, social determinants of health “are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
Today we’ll go over:
- What the different social determinants of health are
- The Healthy People 2030 Framework
- Why SDOH should be a priority for your health plan
- And steps you can take today to address them
What Are The Different Social Determinants of Health?There are several different models of SDOH out there, however, to keep things simple, we’ll distill them into five groups:
- Economic stability
- Education access and quality
- Healthcare access and quality
- Neighborhood and built environment
- Social and community context
These are internal and external stressors that may impact your members’ health, though they aren’t directly related to health. Some specific examples of social determinants of health are
- Water quality or pollution
- Noise levels and housing safety
- Grocery store and fast food restaurant ratios
- Zip code
This has been neatly arranged and explained in the Department of Health and Human Service's new initiatives and plan for 2030, which we will go into more detail about.
The Healthy People 2030 Framework And What You Need To KnowThere are more than 500 data points and objectives that the government has outlined to measure the health of Americans. The goal of these initiatives is to “Create social, physical, and economic environments that promote attaining the full potential for health and wellbeing for all.”
One top-of-mind model of these disparities is the ongoing COVID-19 pandemic. Not all pandemic care is created equal. Millions of family caregivers are unable to access the care that they need while balancing work and care responsibilities, while many older adults are sequestered in long-term care settings unable to see loved ones.
This isn’t just a trend or buzzword—it’s a new evolution of care that’s taking flight. CMS even issued a roadmap for states to address SDOH through value-based reimbursement in 2022 for Medicaid and CHIP (Children’s Health Insurance Program) programs.
One of the more startling truths they shared was: “The United States spends more on health care than almost any other country yet often underperforms on key health indicators including life expectancy, reducing chronic heart disease, and maternal and infant mortality rates.”
In order to stand out and differentiate your health plans from those of other companies, you need to demonstrate a commitment to lowering barriers to accessing needed care. Empower your members to take charge of their own health—without the mess and confusion of the system at large.
Why SDOH Should Be A Priority For Your Health Plan
We sat down with Michael Newell, the owner of Lifespan Care Management, and former nursing school instructor, who has a wealth of experience seeing first-hand the impact of social determinants of health:
Why are there large disparities in how healthcare spending is spread out across populations?
“If you’re managing a population, the 80/20 rule comes to play here. 10-20% of your subscribers account for 80-90% of your actual costs, everyone else is fine. You want to have a strategy to address that 10-20%. In certain populations it’s even worse, 1% can be 30% of the costs.”
Why haven’t SDOH historically been addressed? How does cost play into that?
“When you pay attention to [the cost], SDOH is a big issue: housing, safety, access to care, access to food, social support, things like that. That is opposed to the training of physicians (you don’t want to ask them anything other than symptoms) so what are we doing here? Modern American medicine has modern strategies to address symptoms but not the cause. If we don’t address the cause, we’re not going to have a chance for a cure or appropriate care. Appropriate in my mind, is what actually works:
- What interventions and care strategies actually solve the problem?
- Which medications actually solve the problem?
We have a lot of care that is inappropriate, which is why we’re spending so much money on care because it addresses symptoms and not the problem.”
How could improved physician training work to address SDOH?
“If we have a sense of what factors are getting in the way of stabilizing health problems, identify the 10-20% that have chronic health problems. We’re not addressing symptoms because we don’t know the full problem. Doctors haven’t been socialized to find out what’s behind the problem and the issues that arise when people come in seeking care.
Today’s scenario:
Patient: I have pain.
Doctor’s response: Let me give you some pills.
What doctors should instead be asking:
- How does it happen?
- When did it first start?
- Do you have a history of pain?
When it comes down to it, the experience of pain has a lot to do with what’s going on in someone’s life, even at an early age. The federal government has opened up coding for SDOH so that providers can actually get paid to address these concerns because they’re aware that these are important issues, and they have been largely ignored in the past.”
How does language play a role in health outcomes?
If you really listen to that person (which along the way, they’ll identify their SDOH that are getting in the way of their normal functioning role) the SDOH will manifest itself in terms of symptom etiology and ability to self-care, engage in treatments, and follow instructions.
What we’re saying when a patient isn’t ‘compliant’ is that it infers that they don’t want to get better, they don’t want to do the right thing. They want to do the right thing, and they want to be liked and respected by their provider. If we have an attitude of 'they’re noncompliant,’ and that’s not helpful for anyone.
They’ll pick up on that attitude and decide if they want to fill that prescription. I like the term adherent because it doesn’t connote the blame on the patient. When people aren’t adherent, they might not understand the import of the instructions for various reasons, or they ran out of bandwidth, or perhaps you wrote it down in a way that they can’t understand or recall how to take a medication.”
Newell urges health plans to play an active role in managing benefits. Make sure that treatments that members receive are in their best interest, and are explained to them in a way that they understand.
TIP: Invest in community health workers, and train them in SDOH, to laser focus on your members, with a special focus on high-risk populations to layer in preventative care measures, before small concerns turn into expensive ER visits.
“We have a lot of care that is inappropriate, which is why we’re spending so much money on care because it addresses symptoms and not the problem.”
What Steps You Can Take Today To Improve Your Members’ SDOH
CMS is recognizing the outdated nature of fee-for-service payment models and has shifted toward value-based reimbursement models for many essential healthcare services. This means that you are going to be subject to this in the not-too-distant future.
Today, we’re going to share a few tips on how you can incorporate social determinants of health into your members’ plans today:
Make a commitment to be data-driven in your decision-making.
The most important step in understanding the SDOH of your members is to identify that they exist and in what ways. When you can point to these disparities and address them head-on, you’re acknowledging the imperfections of the current system. Then, you can begin taking steps to solve these problems and bridge the gaps that exist.
Lower the cost of care by taking care of your members' unmet needs.
Stress, for example, is a leading cause of ill-health across the lifespan. A publication from the CDC warns us about the link between childhood stress and chronic disease in later life. When you connect members to providers, remember that you’re not just administering a treatment. You are improving health outcomes; you can’t separate the person from what they’re going through. Remember: patient-centered care means caring for the whole person.
Make sure that your member reviews and feedback systems include SDOH.
When you provide a person with care, you’ve provided one person with care. Healthcare cannot continue to be a conveyer belt of copy and paste care.
Each member’s care needs to be considered within their demographics, their career, their family, and their beliefs. When asking members to assess their experience, make sure that you take their context into account, and demonstrate that you care about them on an inpidual level.
Reminder: Health outcomes are not just tied to direct care, they’re also affected by diet, exercise, along with social and economic factors.
Moving Toward SDOH Is A Step In The Right Direction.Social determinants of health are a great way to assess your plans for efficacy and health equity. By following these tips, you’ll be able to make sure that your members are taken care of from head to toe.
One solution that can help you streamline social determinants of health with your members and their plans, is by checking out our SDOH solution. Lean on a data-driven approach that improves the efficiency of your front-line clinicians.
Which one of these tips are you looking at trying today?

